How do opioids stop breathing?
Opioids are two-faced drugs. They can be used compassionately to relieve pain, but they are also dangerous by instantly stopping breathing when taken in excess. How can one substance do so much to help and harm at the same time?
Each day, fatal overdose occurs ~130 times in the United States. To combat this pandemic, it is critical to identify the the key neurons that opioids act upon to slow breathing. Recently, we showed that two small clusters of brainstem breathing control circuit, including the breathing pacemaker, are the most critical to slow and stop breathing. Within the pacemaker, just ~70-140 neurons (<5% of neurons) are responsible for opioid sensitivity. Importantly, these neurons have no impact upon pain relieving property of opioids. We are now keen to understand how such a small number of neurons could so drastically slow breathing and how / if they are involved in general breathing and endogenous opioids regulation of breathing.
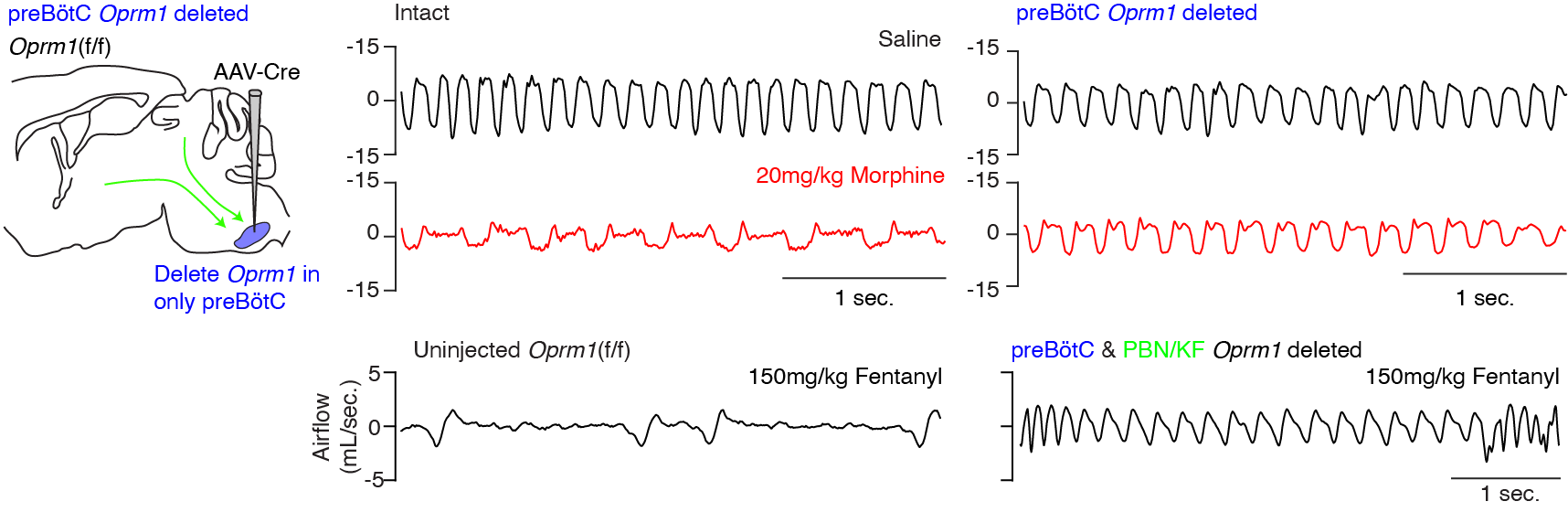
Bachmutsky et. al., 2020 & 2021